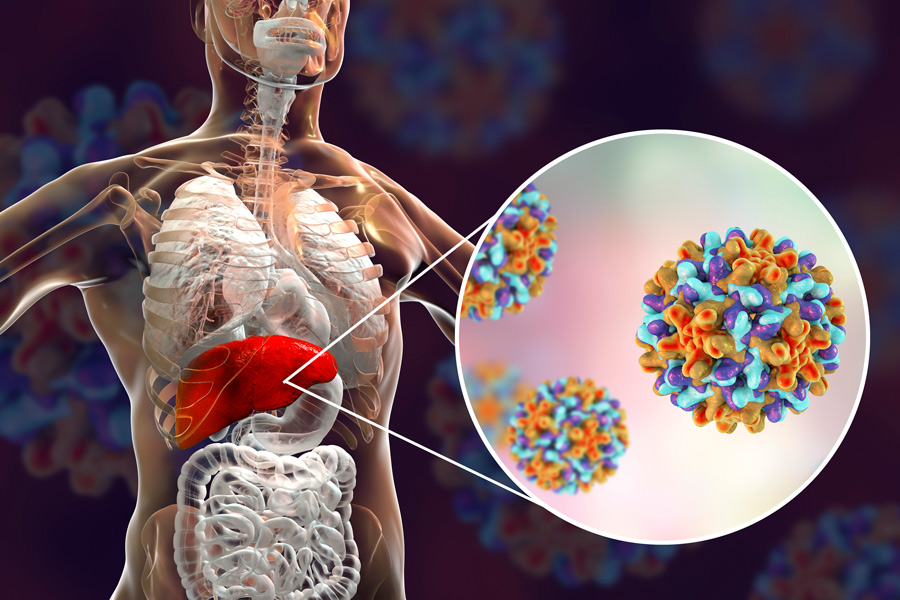
Hepatitis B virus and fatty liver disease are both common conditions which affect the liver, but how these two diseases interact is complex and poorly understood. Dr Wai-Kay Seto and colleagues from the University of Hong Kong have been investigating the influence of fatty liver disease on hepatitis B prognosis using vibration-controlled transient elastography. Their results suggest that high levels of liver fat can worsen the effects of hepatitis B on the liver, but also it can increase the chance of being functionally cured.
Transient elastography is an ultrasound-based technique which can be used to measure liver fat and fibrosis quickly, safely, and non-invasively. It works by measuring the reduction in intensity (attenuation) of the ultrasound scan in liver or fat tissue. As attenuation is greater in fatty tissue (steatosis) than in liver tissue, vibration-controlled transient elastography (VCTE), or transient elastography can quantify liver steatosis as the controlled attenuation parameter (CAP) in units of decibels per meter (dB/m). Liver fat does not slow the ultrasound signal but fibrosis (scarring caused by liver damage) does, and so transient elastography can give a second value known as the liver stiffness measurement, given in kiloPascals (kPa).
Dr Seto and his colleagues at the University of Hong Kong (Queen Mary Hospital) use this technique to investigate how increasing liver steatosis impacts on the prognosis of hepatitis B virus (HBV).

Non-alcoholic fatty liver disease
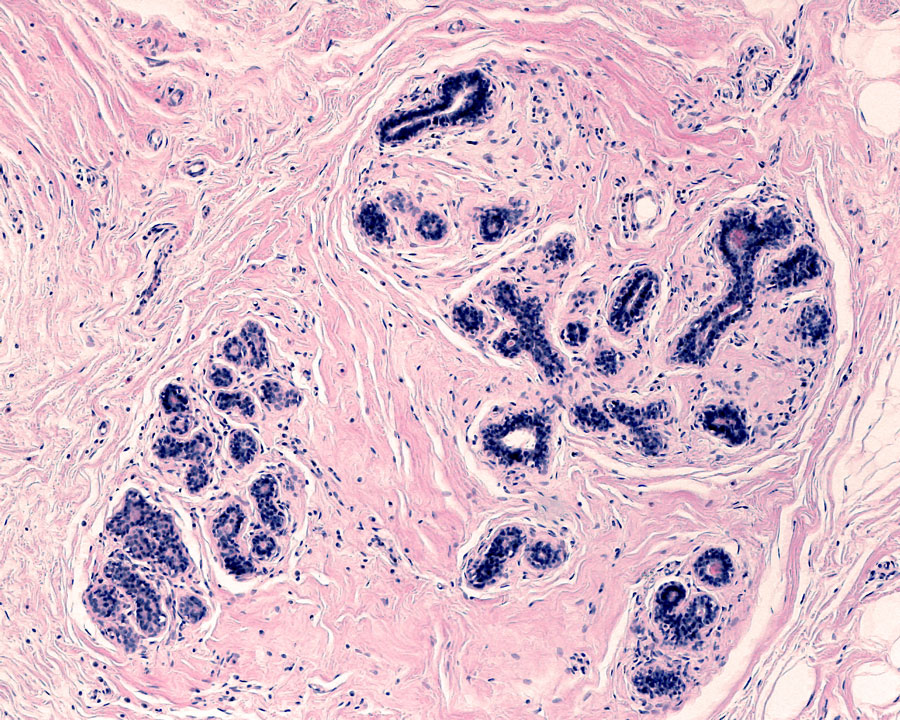
The presence of liver steatosis is often called fatty liver disease, and when not caused by alcohol consumption it is known as non-alcoholic fatty liver disease (NAFLD). NAFLD is a common liver condition, affecting around 24% of the population worldwide and more than 40% of the Asian population. Risk factors for developing NAFLD include diabetes, high blood pressure, obesity, or metabolic syndrome (a combination of the other three risk factors). Left untreated NAFLD can go on to cause liver damage: firstly fibrosis (scarring around the liver), then cirrhosis (scarring and shrinking of the liver) and possible liver cancer. Treatment is weight loss through a healthy diet and exercise, and control of any pre-existing conditions (such as diabetes) that may have contributed to developing NAFLD. Non-alcoholic fatty liver disease can be diagnosed through biomarkers (molecules the volume of which, in samples from blood or tissue, can indicate disease), liver biopsy, or ultrasound – though ultrasound is the most common technique as it supplies immediate results and is a non-invasive procedure.
“…patients with severe steatosis were more likely to also have liver fibrosis, and that this was true for both patients on antiviral treatment and patients not currently receiving treatment.”
Hepatitis B virus
Hepatitis B is an infectious virus spread through bodily fluids, which can cause liver damage if it becomes a chronic condition (lasting more than six months, as determined through blood tests). Chronic hepatitis B (CHB) affects 3.9% of the global population and is more common in those of Asian descent. In adults HBV is usually fought off by the immune system within a couple of months, but if it becomes chronic then the disease can be effectively suppressed with antiviral medications. Antivirals prevent any symptoms or further liver damage, but sometimes may need to be a lifelong treatment as they don’t necessarily cure CHB. Often when the virus is suppressed the liver fibrosis can heal (fibrosis regression), but factors such as obesity and diabetes can increase the likelihood that the liver fibrosis will persist during treatment.
Hepatitis B with liver steatosis
NAFLD is present in a significant proportion of CHB patients (estimates vary from 13.6% to 59.3%), and as other metabolic factors (e.g. obesity, diabetes) impact the progression of CHB it is important to understand if steatosis also affects liver damage from HBV infection. Dr Seto and colleagues performed transient elastography examinations on 1606 patients with CHB and recorded both liver stiffness (fibrosis) and steatosis (as a CAP measurement). They found that patients with severe steatosis (as opposed to no, mild, or moderate steatosis) were more likely to also have liver fibrosis, and that this was true for both patients on antiviral treatment and patients not currently receiving treatment.

This doesn’t mean that the antiviral medications weren’t working – over 90% of the on-treatment patients in the study had undetectable levels of HBV in blood tests. Those patients in the study who were not receiving treatment for their CHB had low levels of HBV in blood tests and so are not thought to require antivirals. Additionally, though severe steatosis increased the likelihood of fibrosis, the impact was different between on-treatment and not-treated patients. For those not receiving treatment for CHB, each increase of 10 dB/m in the CAP measurement (for liver steatosis) was associated with an increase in risk of fibrosis by 15%. In contrast, for patients on antiviral treatment for CHB each increase of 10 dB/m was associated with around an 8% increase in risk of fibrosis.
Follow-up examinations for three years after the initial measurements were taken confirmed that persistent severe steatosis was significantly associated with a higher risk of fibrosis progression in patients not receiving treatment for CHB, and that resolved steatosis was associated with fibrosis regression.

\
Steatosis may increase CHB functional cure
Hepatitis B surface antigen (HBsAg) is the marker on the surface of the hepatitis B virus that is detected during a blood test. HBsAg seroclearance (when the virus is no longer detectable) is considered a “functional cure”, and is uncommon in patients with CHB. Dr Seto and colleagues measured HBsAg levels (and steatosis as CAP measurements) in 330 patients with CHB who were not receiving antiviral medication (due to low levels of HBV indicating that they don’t require treatment) every six months for three years, and defined HBsAg seroclearance as no detectable HBsAg in two measurements taken six months apart. They found that the presence of liver steatosis increased the likelihood of HBsAg seroclearance within three years.
The overall rate of HBsAg seroclearance observed in the study was higher than the average for CHB patients due to the patients selected being those with low virus levels (and therefore already more likely to achieve seroclearance). However, it is not clear why liver steatosis would have the positive effect of making the functional cure more likely. It is suggested that the altered metabolism caused by the presence of liver fat could lead to viral replication being inhibited, and therefore the reduction of HBsAg levels.
“Further research is needed to understand the relationship between liver steatosis and HBsAg seroclearance before any recommendations for patient treatment can be made.”
Future CHB treatment
Only severe steatosis (defined as a CAP measurement greater than 280 dB/m) affected the likelihood of liver fibrosis, but that this is true for both on-treatment and not-treated patients is important for future care of CHB patients. For patients receiving treatment for CHB this means that it may be necessary to also recommend lifestyle changes to combat fatty liver before fibrosis regression can occur, and those patients not receiving treatment due to low HBV levels may still be at risk for fibrosis if they have severe steatosis.
Further research is needed to understand the relationship between liver steatosis and HBsAg seroclearance before any recommendations for patient treatment can be made. Dr Seto and colleagues suggest that further long-term follow-up with these patients, using transient elastography to monitor steatosis and fibrosis, could provide more information and help to advise the prognosis for those with chronic hepatitis B and fatty liver disease.
Yes. Fatty liver disease is common, and there is increasing evidence that elements of fatty liver disease can impact on the disease course of chronic hepatitis B. Regular assessments are especially important in patients with metabolic risk factors (e.g. obesity, diabetes) as the risk of severe fatty liver disease will also increase. Transient elastography is a simple and non-invasive investigation that is both accurate and reproducible, and can provide valuable information in the prognostication of patients.
References
- Seto, W.K., Hui, R.W.H., Mak, L.Y., Fung, J., Cheung, K.S., Liu, K.S.H. Wong, D.K.H., Lai, C.L., and Yuen, M.F. (2018). Association Between Hepatic Steatosis, Measured by Controlled Attenuation Parameter, and Fibrosis Burden in Chronic Hepatitis B. Clinical Gastroenterology and Hepatology, 16: pp. 575–583. Available at: https://doi.org/10.1016/j.cgh.2017.09.044 [Accessed 26 Nov 2020].
- Mak, L.Y., Hui, R.W.H., Fung, J., Liu, F., Wong D.K.H., Cheung, K.S., Yuen, M.F., Seto W.K. (2020). Diverse effects of hepatic steatosis on fibrosis progression and functional cure in virologically quiescent chronic hepatitis B. Journal of Hepatology, 73: pp. 800-806. Available at: https://doi.org/10.1016/j.jhep.2020.05.040 [Accessed 26 Nov 2020].
10.26904/RF-133-5457
Research Objectives
Dr Wai-Kay Seto’s translational and clinical studies are centred on hepatitis B virus and fatty liver disease.
Funding
- SK Yee Medical Foundation Grant, Hong Kong
- State Key Laboratory for Liver Research, The University of
Hong Kong - Outstanding Young Researcher Award, The University of Hong Kong
Collaborators
Research colleagues from the University of Hong Kong who are co-authors of the research articles, and especially Prof Man-Fung Yuen, my research mentor.
Bio
 Dr Wai-Kay Seto is a Clinical Associate Professor in the Department of Medicine, the University of Hong Kong. He is also Assistant Hospital Chief Executive (Research) of the University of Hong Kong-Shenzhen Hospital. He has published more than 190 journal articles and book chapters, the majority related to chronic liver diseases.
Dr Wai-Kay Seto is a Clinical Associate Professor in the Department of Medicine, the University of Hong Kong. He is also Assistant Hospital Chief Executive (Research) of the University of Hong Kong-Shenzhen Hospital. He has published more than 190 journal articles and book chapters, the majority related to chronic liver diseases.
Contact
Wai-Kay Seto
Department of Medicine
The University of Hong Kong Queen Mary Hospital
Queen Mary Hospital
102 Pokfulam Road
Hong Kong
E: wkseto@hku.hk
T: +852 22556979
W: https://medic.hku.hk/en/Staff/University-Academic-Staff/Dr-SETO-Wai-Kay,-Walter/Dr-SETO-Wai-Kay-Walter









