- Chronic headaches are extremely debilitating conditions which significantly impact the quality of life.
- Common causes include migraines, cluster headaches, and occipital neuralgia.
- There are many patients who do not respond to drug treatments or are adamant about making improvements to their lifestyle beyond medications.
- Dr Giorgio Pietramaggiori and Dr Saja Scherer of Global Medical Institute, Switzerland employ minimally invasive treatments such as targeted Botox injections, surgical release of nerves, and fat transfer.
- These treatments aim to offer relief for people suffering from chronic headaches when pharmacological alternatives fail.
Migraines are not simple headaches. Flashes of lights or blind spots, tingling sensation on one side of the face may precede a headache so bad that it can interfere with your normal life for hours or even days. This is migraine. This debilitating form of chronic headache can cause an intense, throbbing pain, usually on one side of the head.

Migraine is a common condition, occurring in about one in seven people globally and with one in four households affected. Interestingly, migraine is more common in women than men, with the reported lifetime prevalence being 33% and 13%, respectively. This may be due to hormonal differences between sexes, with some women more likely to experience a migraine around menstruation. Occipital neuralgia (ON), on the other hand, is more mechanical and less related to hormonal changes. The pain in this disease is often continuous starting in the back of the neck and irradiating the back of the scalp and sometimes felt behind the eyes. At the Global Medical Institute, Switzerland, Dr Giorgio Pietramaggiori and Dr Saja Scherer are on the quest to find minimally invasive treatments for both migraines and ON.
Treatments for migraines – can Botox help?
Drug treatments fall into two main categories. The first treatment aims to treat pain either after or just before the onset of a migraine. The second is taken regularly to reduce the frequency and intensity of migraine headaches (also called disease-modifying medications). Typically, triptans are the drug of choice to stop a migraine attack which are effective for more than half of patients. Other pain-relieving drugs include paracetamol, ibuprofen, opioids, or other analgesics, or anti-inflammatory drugs.
There are some people who take medications and improve their lifestyle, but the impact of migraines is still so debilitating that it reduces quality of life.
The use of these drugs can have long-term side effects, such as dependency, medication-induced headaches, and the development of gastric ulcers with ibuprofen, or constipation with opioids. Preventative medications include anti-epileptics, anti-hypertensive drugs, beta-blockers, and anti-depressants. Lately, antibodies against CGRP (calcitonin gene-related peptide, a molecule expressed during migraine) have been introduced as a disease-modifying treatment to reduce the burden of this disease.
However, these drugs are not suitable for everyone. There are some people who take medications and improve their lifestyle with diet, sleep, and stress management, but the impact of migraines is still so debilitating that it severely reduces their quality of life. So, what are the options for these people?

Botox (botulinum neurotoxin) has been used to improve migraine symptoms for extended periods without pharmacological side effects. Botox is administered via microscopic injections in the zone of pain of migraine, following well-established protocols which are adapted to each particular situation, and are usually effective for up to 12 weeks. When this approach works, patients regain pain-free days and reduce the use of drugs, in turn reducing their side effects. Sometimes, depending on the type of migraines, patients under the effects of Botulinum toxin are completely migraine-free. However, some conditions are less responsive to Botulinum toxin injections, for instance, occipital neuralgia.
What is occipital neuralgia?
Occipital neuralgia (ON) or Arnold’s neuralgia is another form of chronic headache caused by inflammation of occipital nerves. Occipital nerves are the structures that give sensation to the back of the head. Along their trajectory, these nerves can be pinched by the large muscles of the neck and shoulders that insert into the skull like the trapeze muscle. ON is commonly confused with migraines or cluster headaches due to the similarity in symptoms, but they can also often occur together.
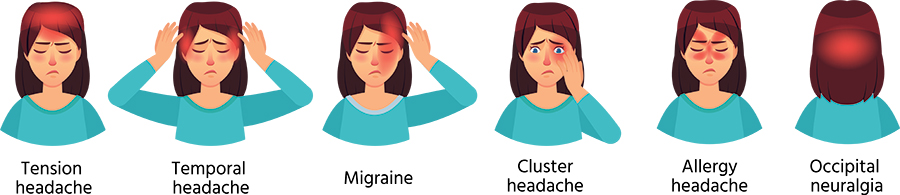
ON symptoms include shooting pain in the back of the head, with hypersensitivity of the scalp (burning or electric sensation) as well as behind the eyes. Since it is caused by the mechanical irritation on the occipital nerves, pain is usually felt most of the time with attacks of higher intensity. Due to the frequent overlap of ON with migraines, the prevalence in the population remains unclear. But it is certainly believed to be a consequence of modern lifestyle, such as long hours spent in front of computers or smartphones.
Treatments for occipital neuralgia
Despite the condition being well-characterised, ON is often misdiagnosed and mistreated as it does not respond to migraine treatments. If the symptoms do not improve with standard medications, a topical infiltration in the pit between the muscles of the back of the head, usually identified as the starting point of the pain by the patients and corresponding to the zone of nerve compression, will improve the ON at least temporarily. This injection confirms the diagnosis of ON and opens the way to surgical decompression, if needed.

Drs Pietramaggiori and Scherer present a minimally invasive surgical intervention to decompress the occipital tension. The surgical technique releases the compressed nerves and blood vessels located in the back of the scalp using a small incision (usually between 2.5 and 3.5cm). The procedure can be performed under both general and local anaesthesia, depending on the individual situation. The impact of the procedure was determined retrospectively by assessing reduction in the number of headaches that participants experienced per month and the pain they reported as well as more quantitative methods, such as the amount of medication used for pain following the procedure.
A significant decrease of 50% of headache was found in 91% of patients, with a staggering 45% of ON patients reporting that their occipital symptoms completely stopped. All other measures of pain – including drug use, days with pain per month, and chronic pain intensity – were reduced by at least 70%. An additional positive outcome was that only minor complications were reported, such as scar issues, in a small number of patients. Based on these results and the increasing number of patients coming to Switzerland to receive this surgery, Drs Pietramaggiori and Scherer hope that this minimally invasive decompression technique becomes the front-line treatment for patients with ON.
Drs Pietramaggiori and Scherer report the effective use of autologous fat transfer for the treatment of occipital neuralgia and migraines.
The future of headache treatments
Drs Pietramaggiori and Scherer also report the effective use of autologous fat transfer for the treatment of ON and migraines. In particular, this approach is effective in patients bearing post-traumatic or post-surgical scar tissue. They have found that fat tissue reconstitutes the anatomy of the skin, reducing compression, tension, and irritation of nerve branches. Injection of fat from elsewhere in the body is a simple and effective treatment for pain. With their continued research, Pietramaggiori and Scherer are hopeful for a future with even less invasive treatments for migraine, cluster headaches, and ON.

In our practice, about half of the patients with migraines can be satisfactorily managed with Botulinum toxin for extended periods of time. Often, after months or years of treatment, patients ask to be operated, if possible, to achieve a permanent improvement without the need for recurrent injections. Botulinum toxin injections are also used as tests to evaluate whether a patient could benefit from a minimally invasive decompression of nerves around the head to improve their migraines.
Why do some people not respond to drug treatments for headaches?
There are several reasons why patients may not be satisfied with drugs for their headaches. If the migraines are too frequent, requiring an almost daily use of triptans, the drugs start to lose their efficacy, the need for them increases, and the burden of side effects rises to the point that patients may develop headaches from them.
There are also patients who have other medical conditions (vascular or cardiac issues) and may not be eligible for the use of migraine drugs, such as triptans.
In addition, some headaches, typically ON, have a mechanical origin and respond only marginally to medications, as the compression on the nerves must be released to stop the pain.
Do you think there is a possibility for these minimally invasive procedures to become the standard treatment or will drug treatment always be tried first?
In our opinion, drugs will be always attempted first, and for a number of patients, they will achieve the intended goal of allowing a normal life. In selected cases, like patients with occipital neuralgia or refractory or chronic migraines, a surgical approach will likely become the preferred approach as drugs are not effective for nerve compression syndromes. For these cases, we envision that minimally invasive surgical decompression will become the gold standard and preferred treatment. We see the analogy with carpal tunnel syndrome where surgical decompression is the preferred approach once the diagnosis is confirmed.