- Traumatic brain injury remains a major cause of disability and death worldwide.
- Timely detection of the injury could lead to early intervention and save lives.
- Current diagnostic methods are expensive, non-portable, and time-consuming to apply.
- Professor Pola Goldberg Oppenheimer at the University of Birmingham, UK, has developed a novel handheld device that helps detect and classify brain injury by scanning the back of the eyes.
Traumatic brain injury (TBI) is an injury to the brain caused by sudden shock or impact to the head. Usual causes include road traffic collisions, assaults, falls, and accidents at home, work, and during contact sports. Severe TBI can lead to permanent disability and even death. This is why detecting it early after the incident is crucial for timely medical and surgical interventions that can prevent TBI-related disability and death.

Most of the acute damage to the brain after a traumatic injury occurs immediately after the event. Taking the injured individual to the nearest hospital to undergo a head scan can cause a significant delay in the TBI diagnosis, with detrimental consequences for the injured individual and their family. Moreover, many hospitals do not have the appropriate facilities for urgent brain surgery, which means the patient would have to be moved to another hospital, causing further delays.
So far, no sensitive and portable technology is available to identify brain injury in the field, for example at stadiums during sports events or at the roadside after motor vehicle collisions.
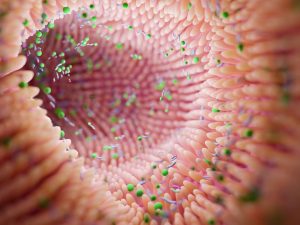
The retina and optic nerve share most of the brain’s biochemical properties – this way, they provide a ‘window’ into the biochemistry of the brain.
To address this lack of technological means for the early detection of TBI, Pola Goldberg Oppenheimer, a Professor in Micro-Engineering and Bio-Nanotechnology at the University of Birmingham, UK, has developed a groundbreaking laser-based, eye-safe device (EyeD) technology. This technology can detect molecular changes that reflect brain damage by scanning the back of the eye with a handheld device.
Window to the brain
Professor Goldberg Oppenheimer and her team had previously shown that they could detect changes to experimental animals’ brain chemistry after an inflicted injury by using Raman spectroscopy. Raman spectroscopy is a scientific method where scattered light is used to identify and quantify specific chemical components in a sample – in this case, specific molecules in the brain that work as TBI markers.
These molecules are brain-specific lipids and biochemicals such as cardiolipin and cytochrome C, or brain-specific neuromarkers such as S100B, glial fibrillary acidic protein, and N-acetylasparate (NAA). Injury to the head causes the levels of these markers to change, indicating that something is wrong. Changes in these markers not only reflect brain damage but can also provide information about the brain damage type and severity. The measurable marker levels and their combinations are the base for the specialised software to construct what the team calls molecular fingerprints, specific marker combinations that reflect certain types of disease or injury.

Modified from Banbury, et al, (2023), doi.org/10.1126/sciadv.adg5431
Detecting molecules in the brain would typically require an invasive procedure. However, the researchers thought of a method to get the relevant information in a painless and non-invasive way. They applied the Raman spectrometry method at the back of the eye (fundus), where the retina (the innermost layer of the eye) and the optic nerve (the nerve that transmits visual information from the eye to the brain) are located. The retina and optic nerve are both structurally an extension of the brain itself and therefore share most of its biochemical properties – this way, they provide a ‘window’ into the biochemistry of the brain.
How does it work?
EyeD is a portable, non-invasive, laser-based device that uses spectroscopic eye-safe technology – meaning it doesn’t use radiation that could harm the eye. The device uses a smartphone fundus camera and flash for the imaging and illumination of the retina. It then detects and analyses the composition of the specific neuromarkers, picking up the slightest changes in their levels, and creates specific molecular fingerprints. With the help of a specially designed AI and an advanced statistical tool called SkiNET (artificial neural network algorithm of the self-optimising Kohonen index network), the device can use these fingerprints to successfully classify the TBI and help accurately measure the damage.

Modified from Banbury, et al, (2023), doi.org/10.1126/sciadv.adg5431
To test their invention further, the team conducted an experiment on pigs which were given traumatic brain injuries in the humane form of electrical stun shocks directly to the brain. These were followed by the slaughter of the animals following the United Kingdom Food Standards Agency (UK FSA) health guidelines as per standard slaughtering practice. The eyes of these pigs, along with eyes from healthy pigs that died from natural causes, were scanned two to four hours after extraction and all results were then analysed using the AI and SkiNET tools. Similar experimentation was performed on rodents.
EyeD is a low-cost, handheld device that can be used to assess patients in the field immediately after the injury occurs.
The results of both these experiments confirmed that by using this novel method, the team could accurately tell apart the eyes of the injured animals from the eyes and retinas of the healthy ones (control group), but also efficiently classify the different eyes and retinas according to level of brain damage.
Point-of-care neurodiagnostics
EyeD is a low-cost, handheld device that can be used to assess patients in the field immediately after the injury occurs. The device itself is non-invasive and easy to use as part of the initial assessment by paramedics or other front-line clinicians.

Modified from Banbury, et al, (2023), doi.org/10.1126/sciadv.adg5431
Its precision can provide the user with valuable information on the presence and severity of the brain injury at an early stage and allow them to make safe decisions on whether the injured person requires medical or surgical intervention in a dedicated facility without any unnecessary delays.
What inspired you to conduct this research?
I am a Biomedical Engineer specialising in developing cutting-edge solutions to important medical problems. Realising that TBI is a leading cause of morbidity and mortality worldwide and is becoming one the major challenges of the 21st century has inspired me to conduct this research.
While life-changing decisions must be made rapidly, TBI is notoriously hard to diagnose at the point-of-care, resulting in incorrect patient management. The chances of an individual suffering cognitive or physical impairment are massively increased. With millions affected annually, the burden that TBI imposes on society makes it a pressing public health and medical problem.
Current diagnostic methods are woefully inadequate, either requiring large equipment, long-waiting times, being highly invasive or not sensitive and timely enough. Point-of-care technology for TBI does not currently exist. Therefore, there is an urgent need for new technologies to achieve timely intervention through rapid and accurate diagnostics at the PoC. This was the major drive behind this research.
Are you planning human trials to develop the technology further?
We are currently optimising the prototype for clinical validation of Raman-fundus spectroscopy, engineering a user-friendly deployable device that is integrated with our artificial neural network algorithm for an automated interpretation of outputs without requiring specialist support. This device is able to rapidly classify spectral data and clinically evaluate device usability in healthy volunteers and in patients to demonstrate its potential for real-time diagnosis. After establishing device tolerability and usability, we are proceeding to a first-in-human evaluation and small-scale clinical trial.
Do you intend for the 3D printing design and software to be open source to allow access and low-cost manufacturing in less privileged countries?
Absolutely. TBI incidence continues to rise in all age groups, particularly in low- and middle-income countries (LMICs), where 90% of global trauma cases occur. Further, LMICs, where a family must often sell assets to pay for a CT, would benefit significantly from this technology, including if this was used for monitoring TBI evolution in poorly resourced environments
How are you planning to make the relevant institutions such as sports clubs and health boards aware of the benefits of EyeD and how would you eventually introduce it to them?
To ensure the maximum benefits to patients, we have already been conducting this research in partnership with local hospital and pre-hospital care providers, as well as sports teams. This started the process of dissemination to end-users whilst involving them in strategy and design. To ensure that we target this new technology at the most important medical need, clinicians at the Queen Elizabeth Hospital Birmingham along with members of the public have input into the development and translation of the technology, enabling the design of the various technology components to be optimised and tailored to deliver the greatest benefit to patients. To enable the translation and acceptance of our technology, we will further engage with all stakeholders, including patients, commercial partners, and sports organisations.
We have been creating the following dissemination outputs:
• Short awareness animations on TBI, diagnosis, and EyeD, suitable for those with brain injury;
• Events with local sports groups:
– Short talks with Q&A from researchers and others, eg, sport concussion group
– Hands-on family-friendly activities on prevalence and signs of concussion
– Perception and opinion gathering from wider public on future research
Could you think of any other potential applications that SkiNET can have in future?
It can be further exploited for research and development of new pathways to optimise resolution and optical throughput. Samples, such as hydrogels and artificial cerebrospinal fluid, could be studied with model markers. It could be particularly useful for animal and human model studies and contribute towards the development of new means to identify changes in brain biochemistry or function due to either acute or chronic neurological diseases such as Stroke, Alzheimer’s, etc.
In the field of Raman spectroscopy and even more generally in chemometrics, principal component analysis (PCA) is favoured for projection and feature extraction, followed by partial least squares discriminant analysis and, more recently, deep-learning models for classification. However, PCA routinely shows poorly defined class boundaries, struggles with large intra-class variance (such as biological samples) and quickly breaks down for multi-class problems. Furthermore, classification is often handled in isolation to projection and feature extraction, forming a semantic disconnect, and whilst deep learning has shown impressive classification results, these methods offer no insight into the underlying physical and chemical changes.
Our aim with SkiNET was to provide a single method to address each of these stages, connected by a single mathematical principle and improve on the issues found using PCA-based approaches.
We developed an improved self-optimising discriminant index based supervised learning method, defined as the self-optimising Kohonen index network (SKiNET) to demonstrate effective classification, and illustrated the complete linked workflow from projection to classification by means of a user-friendly web app. This represents a major shift that follows a growing trend in industry to move from traditional desktop applications to the cloud (including office suites, multimedia editing, and computer aided design) and yet the advantages of connected scalable applications are seldom leveraged in the scientific community.