The future of bionic limbs
- Health & Medicine
Artificial limbs are essential to improve the quality of life of people living without limbs. Bionic limbs such as bone-anchored prostheses use implants directly inserted into the living bone for more stability. However, this technology still causes adverse events. Dr Laurent Frossard, Adjunct Professor of Bionics, and Professor David Lloyd, Professor of Biomechanical Engineering, combine biomechanics and computational modelling to develop a new integrated, wearable and non-invasive diagnostic device relying on the design of a digital twin of the residuum, which may ultimately improve the quality of life of people suffering from limb loss.
Over 2.2 million Americans are currently living with limb loss, and this number may double by 2050. The main causes of amputations are disease (such as diabetes) and trauma (car accidents or military conflicts). Limb amputation requires a lifetime of care. For each amputation, the cost of prosthetic care has been estimated to range between $1.4 and $2.8 million over a lifetime.
The everyday use of artificial limbs is critical to the wellbeing of these individuals. Orthopaedic surgeons, rehabilitation specialists and prosthetists work together and make bespoke recommendations with the intention to maximise comfort, stability and mobility of prosthetic fittings. However, this is not without difficulty.
Challenges of current prosthetic attachment
Prosthetic fittings that allow sustained high-levels of daily activities are difficult to achieve. Indeed, skin, nerves, muscles and bones of the residuum (also called the stump) may be compromised by acute and chronic skin issues, oedema, neuroma, muscle contractures, or fractures. This makes daily prosthetic loading difficult to withstand. Moreover, sockets are challenging to fit around stumps with incongruous shapes. Patients living in hot conditions are particularly disadvantaged because perspiration due to heat and humidity makes sockets difficult to wear. Challenges with prosthetic fittings lead to frequent and, too often, permanent prosthesis abandonment in 25–57% of cases.
Role of bionic solutions
Alternatively, individuals experiencing overwhelming socket issues can be fitted with bionic limbs. A bionic solution is a technological platform relying on three interconnected pillars: the engine, the chassis, and the power-assisted steering wheel.

Advanced prosthetic components (the engine), such as microprocessor-controlled robotic-like artificial joints, are the central part of bionic solutions. Suitable attachment to the residuum (the chassis) can be achieved through direct skeletal attachment using osseointegrated implants, rather than a socket. The inner part of the implant is inserted into the living bone. The outer part protrudes from the skin of the residuum, enabling external attachment of the bone-anchored prosthesis.
Intuitive control of advanced components (the power-assisted steering wheel) can be achieved using sensors harvesting physiological signals from the brain, nerves or muscles. Bionic limbs therefore have physical connections with all sorts of body parts like the brain, nerves, muscles, skin and bone.
The digital twin of the residuum is a virtual replica living inside the computer.
Strengths of bionic limbs
Promising life-changing benefits of bionic limbs showed by long-term efficacy studies are compelling for patients. The direct attachment of the prosthesis through an osseointegrated implant has immediate benefits. It eliminates all typical burden associated with a socket, particularly the residuum’s skin problems. It eases attachment and removal of the prosthesis. It also provides a much more comfortable sitting position and allows a much larger range of movements.
There is overwhelming evidence that bionic limbs attached to osseointegrated implants significantly improve mobility. Users walk faster for longer bouts of daily and recreational activities. This is especially obvious for young and active individuals. Users of osseointegrated implants report that they feel that their prosthesis is more like a part of their body; they experience a phenomenon called osseoperception. Practically, they can feel more vibrations. This helps to feel where the prosthetic foot is on the ground and the type of surface the person is walking on. Dr Frossard has published studies showing that when compared to typical socket prostheses, bone-anchored bionic prostheses significantly improved quality of life by about 17%.
Weaknesses of bionic limbs
Occurrence and severity of adverse events with bone-anchored bionic prostheses are yet to be fully resolved. Bionic limbs can potentially cause issues with implant stability, bone fracture, breakage of the implant parts and infection. All these adverse events have several common negative effects. They cause pain. They significantly disturb the lifestyle because they limit usage of the prosthesis for prolonged duration. They also cost money paid either by the healthcare system or the users themselves as out-of-pocket expenses.

A need to improve
Efforts must be made to lessen severity and incidence of adverse events of bone-anchored bionic prostheses. Prostheses must become safer and more accessible to a large population worldwide. Significant reduction of the risks is a prerequisite for unequivocal approval from international governing bodies such as the FDA. Safer treatment will also warrant a more successful development of the next generation of brain-activated neuroprostheses.
A new radical approach
Dr Frossard and Prof Lloyd believe that one way to address the current shortcomings of bone-anchored bionic prostheses is to have a radical new approach relying on the design of a ‘digital twin’ of the residuum, to assess residuum health under real-life conditions. Indeed, adverse events primarily depend on residuum health, which is usually assessed through physical examinations, medical tests and imaging modalities. This is not sufficient to examine the effects of the prosthesis while wearing it.
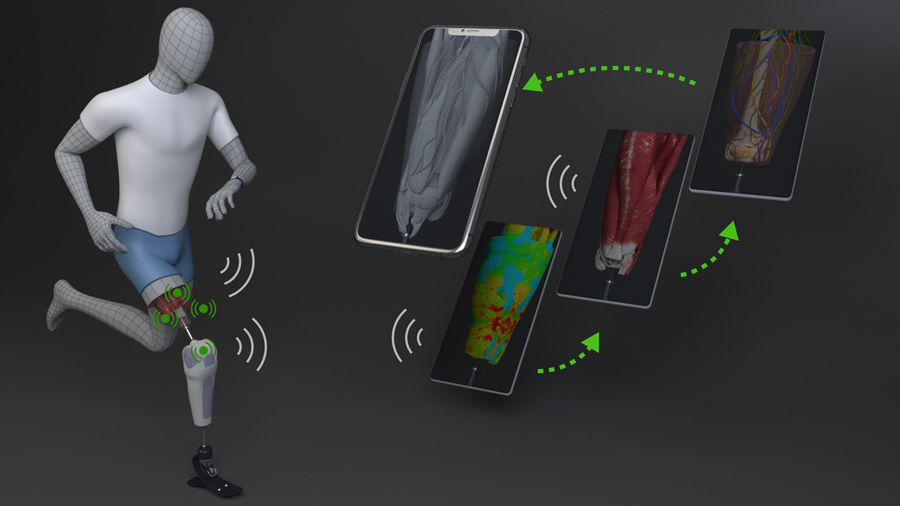
This is why Dr Frossard and Prof Lloyd are currently developing an integrated, wearable and non-invasive diagnostic device. By computing physiological measures related to residuum health and creating a virtual replica (digital twin) of the residuum, the diagnostic device could improve care of patients and facilitate their rehabilitation.
Features of the diagnostic device
Different sensors assess the mechanical constraints applied by the bone-anchored bionics on the residuum and measure the resulting movements of the tissues (bone, muscle, tendon, fat, skin) within the residuum. The back end the device consists of the software integrating all this information into a personalised digital twin of the residuum. Basically, the digital twin of the residuum is a virtual replica living inside the computer. It corresponds to the high-fidelity physics-based model of the different tissues constituting the residuum. The front end of the device consists of a handheld device (such as a smartphone) that provides a visual animation of the model in real time so that patients and clinicians equipped with the device and see can how movements impact the inside of the body.
The diagnostic device provides a radically new and empowering experience for patients.
Improving rehabilitation for patients
The diagnostic device provides a radically new and empowering experience for patients. It can help them monitor how their loading positions stimulate specific zones of the implant in real time using a friendly-user interface and guide them to adopt pain-free positions. By improving stability, it can reduce risks of loosening, fractures and infections. It can also allow patients to better inform clinicians about how a treatment or intervention feels. Altogether, this new approach can increase the quality of life of individuals suffering from limb loss.
Making the unknown visible to clinicians
The digital twin provides detailed personal records on residuum health, osseointegration and adverse events. The diagnostic device therefore creates tremendous opportunities to extend precision medicine: by assisting clinicians in detecting residuum issues during rehabilitation and beyond, it helps them make more accurate decisions. In the long term, the accumulation of data contributes to developing models that can predict adverse events such as unfavourable bone remodelling or elevated inflammatory response.
Reducing healthcare expenses
The diagnostic device could potentially improve cost-effectiveness of bionic solutions by reducing over-prescription when considering care interventions. By improving residuum health, the diagnostic device could also reduce the lifetime financial burden on healthcare system of treatments due to poor residuum health of patients.
Click here to view the image in a separate window
Developing the next generation of bionic limbs
The digital twin enables the simulation of specific effects from a particular intervention before actually doing the intervention. It allows us to predict outcomes and, possibly, anticipate the likeliness of adverse events. It can enable immediate adjustments to residuum loading, stresses and strains, and therefore potentially improve long-term residuum health.
The use of a digital twin is essential to develop intuitive control of advanced components using sensors harvesting physiological signals from the brain, nerves or muscles. The aim is to enable patients to control bionic limbs by merely thinking about the action they want to perform. The diagnostic device can enable safer developments of personalised neuroprostheses by making the link between the command (like the contraction of muscles) and the functions of the prosthesis (such as ascending stairs, grabbing an object).
The digital twin will also allow new neuroprostheses to reverse the current dynamics between the users and their prosthesis. At the moment, despite advances in microprocessors controlling the prosthesis, users must adapt to the functions of their prostheses. With the new neuroprostheses, it will work the other way around: the prostheses will respond to the individual command of the users.
Dr Frossard and Prof Lloyd’s work is essential to opening up access to new bionic solutions, improving safety and mobility as well as, ultimately, improving the quality of life of individuals suffering from limb loss.
To find out more: https://eprints.qut.edu.au/view/person/Frossard,_Laurent.html

What sparked your passion for bionic limbs?
I have always been fascinated by the magic of computers and the mystery of the human body. Bionics is a way to combine these two passions. I feel privileged to work in the field of bionics that can ultimately transform lives of people suffering from limb loss.
References
- Prochor P, et al. (2020) Effect of the material’s stiffness on stress-shielding in osseointegrated implants for bone-anchored prostheses: a numerical analysis and initial benchmark data. Acta Bioeng Biomech. 2020(2):69-81. https://eprints.qut.edu.au/200078/1/2020.pdf
- Frossard, L., et al. (2019) In-vivo kinetic system to sustain residuum health of service members with lower limb loss: From proof-of-concept to digital twin. Military Health System Research Symposium (MHSRS). https://eprints.qut.edu.au/131940/
- Frossard L, et al. (2019) Automated characterization of anthropomorphicity of prosthetic feet fitted to bone-anchored transtibial prosthesis. IEEE Transactions on Bio-Medical Engineering. 66(12):3402-10. https://eprints.qut.edu.au/127745/1/127745.pdf
- Frossard L, et al. (2018) Cost-effectiveness of bone-anchored prostheses using osseointegrated fixation: myth or reality? Prosthet Orthot Int. 42(3):318-27. https://eprints.qut.edu.au/114520/1/Art-QALS-Cost%20Effectiveness-ePrint-06.pdf
- Pizzolato C, et al. (2017) Biofeedback for Gait Retraining Based on Real-Time Estimation of Tibiofemoral Joint Contact Forces. IEEE transactions on neural systems and rehabilitation engineering: a publication of the IEEE Engineering in Medicine and Biology Society. 25(9):1612-21. https://ieeexplore.ieee.org/stamp/stamp.jsp?tp=&arnumber=7903736
- Frossard L, et al. (2013) Load applied on a bone-anchored transfemoral prosthesis: characterisation of prosthetic components – A case study.J Rehabil Res & Devel. 50(5):619–34.https://eprints.qut.edu.au/83145/23/Knee%2Bcomparison%2Bfor%2BOI-ePrint%2B03.pdf
10.26904/RF-134-7477
Research Objectives
The team are developing accurate personalised digital twins of humans and devices that operate in real-time by combining data from laboratory-based instrumentation, multimodal medical imaging and wireless wearable devices. These technologies are being applied to a range of medical diagnostics required for personalised surgical planning, implant design and manufacture, and assistive devices.
Bio

Adjunct Professor Laurent Frossard
Chief Scientist Officer at YourResearchProject
Dr Laurent Frossard is a bionic limbs scientist passionate about developing ground-breaking prosthetic solutions to improve life of individuals suffering from limb loss. He is internationally recognised as a researcher and independent expert for his unique expertise in bionic limbs. He approaches bionic solutions from an all-rounded perspective integrating prosthetic biomechanics, clinical benefits, service delivery and health economics. Dr Frossard has over 25 years of experience both in academia and private industries in Australia, Canada and Europe working with more than 100 organisations worldwide. He is currently the Director and Chief Scientist Officer at YourResearchProject Pty Ltd and Adjunct Professor at the Griffith University, Queensland University of Technology and University of Sunshine Coast in Australia.

Professor David Lloyd BSc, PhD, FISB
Professor of Biomechanical Engineering
David Lloyd is a Professor of Biomechanical Engineering and Director of the Griffith Centre of Biomedical and Rehabilitation Engineering. He has published over 250 full scientific articles (16,300 citations, 66 h-index, Google Scholar), and received over $AUD 34M in research funding with many awards such as the Fellow of the International Society of Biomechanics, 2020 Geoffrey Dyson Award, and The Australian 2019 Biophysics Field Leader. Prof Lloyd and his team develop personalised digital twins of humans for medical technologies to assist surgical planning as well as implant design and neuro-assistive devices.
Contact
PO Box 143, Red Hill, 4059
Queensland, Australia
E: [email protected]
T: +61 4 13795086
W: https://www.laurentfrossard.com/
W: https://www.griffith.edu.au/menzies-health-institute-queensland/disability-and-rehabilitation/gcore

Creative Commons Licence
(CC BY-NC-ND 4.0) This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. Creative Commons License
What does this mean?
Share: You can copy and redistribute the material in any medium or format



A human language-based consciousness model

Robots take ultrasound to the fourth dimension

A career in cancer

Zika Virus and the Rio Olympics: What is the Risk?

Migraines, occipital neuralgia, and cluster headaches

