- Training in paediatric cardiology can be a long and arduous process that is traditionally performed by hands-on practice on patients.
- With new procedures developing and standards of care increasing, it becomes ever more difficult for doctors to get enough cases to train.
- Realistically simulating medical procedures can offer a solution to this problem.
- The 3D lab at the Department of Paediatric Cardiology and Intensive Care at the LMU University Hospital Munich, Germany, has developed a paediatric cardiology training programme that has so far shown great potential.
Congenital heart defects (CHD) are defects in the heart’s structure and present at about 1% of all live births. Such structural abnormalities include defects in the inner walls (septa) of the heart, narrowed, obstructed or additional vessels, stenotic (narrowing) or incompetent heart valves, and combinations thereof. In the past, cardiac catheterisation, the procedure of inserting a wire and flexible tube inside the heart under x-ray vision (fluoroscopy) was only used for diagnostic purposes. Nowadays, catheter investigations also allow for complex treatments; this is called interventional cardiology. In fact, these interventions have in many cases replaced open-heart surgery, since they offer less invasive treatments with great results and minimal complications for the patients.
Aiming for higher standards
Treating congenital heart defects in children not only requires detailed knowledge of the cardiac anatomy, but also intense and continuous training to learn and maintain the high-level skills of handling the catheters and devices. Unfortunately, training opportunities are scarce for reasons of availability but also patient safety.

Could simulation, which has previously given solutions in other areas of medicine and surgery, offer realistic training opportunities for both new and experienced physicians? Carina Hopfner, Marina Nagel, Professor Nikolaus Haas, and their team at University Hospital Munich in Germany firmly believe that 3D model-based training offers unique possibilities to improve technical and interventional skills.
Treating congenital heart defects in children requires intense and continuous training to learn and maintain the high-level skills of handling the catheter.
The researchers have managed to develop a realistic ‘hands-on, patient-off’ simulation training using 3D printed models of both healthy hearts and those with congenital heart defects. The team has recently conducted a study to find out whether simulation-based training can improve the doctors’ knowledge, hands-on skills and understanding of these complex procedures. So far, their results have been more than encouraging.
Designing the simulation model
Hopfner, Nagel, and Haas used anonymised data from previous heart scans of children and adults with CHDs and anatomically normal, unaffected hearts. This data, with the help of a highly specialised medical 3D software (Materialise Mimics Innovation Suite), allowed the team to create models of hearts including their blood-filled chambers and major blood vessels as a precise copy of the real patient’s anatomy. These digital models were then 3D printed.
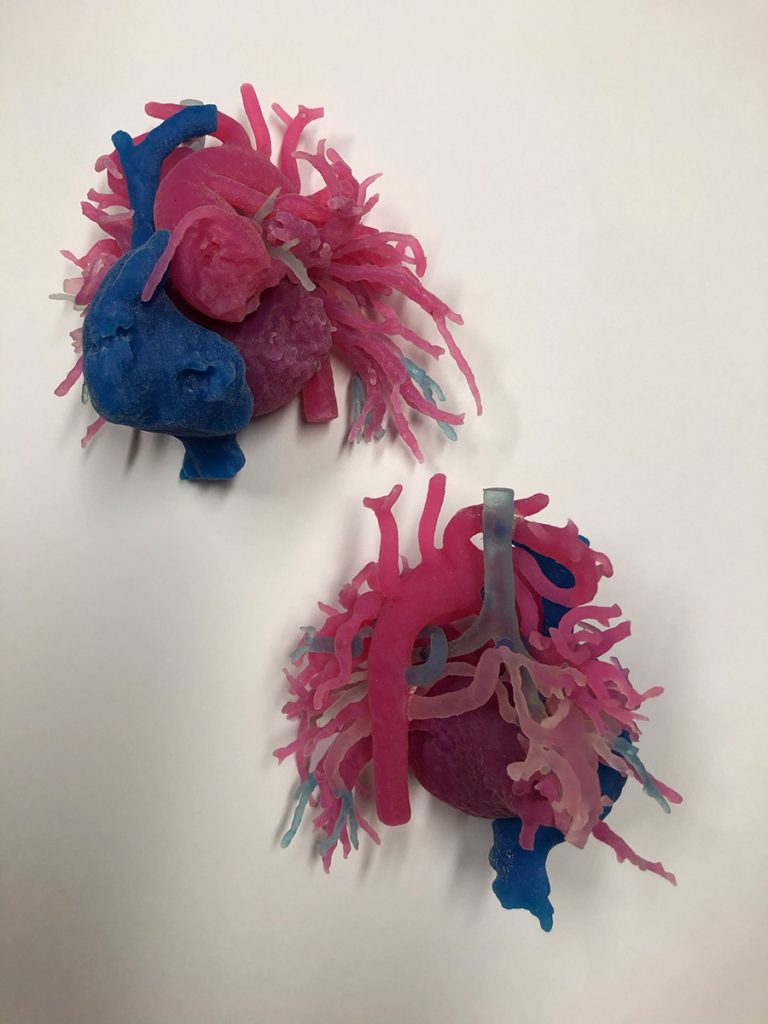
The material used was a soft silicone rubber and a water-soluble support material. The 3D printed heart models were next inserted in baby dolls for a realistic patient experience. The dolls were positioned in the catheter laboratory on the examination table in the same way as a patient. To assess and visualise the position and the anatomy of the heart inside the body, the doll would be scanned the same way real patients are.
The researchers next designed training modules tailored for both new and experienced paediatric cardiologists, as well as for students. 19 participants in total completed the training module and practised all the relevant skills, including catheterising and treating the defective heart models under supervision.
Evaluating the training model
The data collected from the above experiment included the procedural time for all participants and the radiation time the simulated patient had to be x-rayed. At the end, all participants had to fill out an anonymous questionnaire designed for evaluating the training. Finally, the participants could also provide feedback regarding the process by sending free texts.
Participants were encouraged to repeat the procedures multiple times and thereby train the handling of interventions with increasing complexity. The analysis revealed a reduction in the average radiation time from 218 seconds in the first to 104 seconds in the third training task, despite the increased complexity of the simulated intervention. The researchers showed that the radiation times were reduced as the participants gained experience. On the survey, the simulation was rated as very good by the participants (84.2%).

The majority of them also stated that the models were well suited for independent practice and left very positive comments on the overall training experience.
An ongoing and international project
The team has organised additional workshops in Germany and other countries and received positive feedback on their training model. This included a 2019 workshop for paediatric cardiology that took place at Ayder Referral Hospital in Ethiopia. Their Ethiopian colleagues completed a similar training module and practised on heart models before they applied their new skills to actual patients.

During the event, eight children were successfully treated by the Ethiopian doctors under supervision of the German team. The Ethiopian colleagues continued practising their skills after the end of the workshop by using the 3D printed models to maintain and further improve their interventional skills. The German team’s long-term goal is to enable their Ethiopian colleagues to treat CHDs independently; additional workshops in Ethiopia are scheduled.

Since their first study, the team has been working continuously on improving their training models. So far, they have managed to develop patient-specific models that can help doctors improve their catheter skills.
Individualised simulation and training procedures are also feasible to plan a complex procedure by studying ahead the specific patient’s heart structure. Hopfner, Nagel, and Haas have also found a way to produce an anatomical and pathological variety of a single cardiac structure by modifying information from an existing patient’s single scan. Finally, with the use of a connectible pulsating driving unit and a system of silicone tubes filled with water, their latest model can even beat like a real heart, making the training experience much more realistic.
Hopfner, Nagel, and Haas have found a way to produce a variety of 3D structural heart models by modifying information from an existing patient’s single scan.
What happens next?
3D printing for medical training has been successfully used before in paediatric cardiac surgery and other fields of medicine. In this study, however, the researchers were able to demonstrate that their realistically created 3D heart models can be used effectively and safely by doctors to train cardiac catheterisation under realistic conditions. Their model offers a training platform that allows a sustainable, reproducible and stress-free ‘hands-on, patient-off’ training experience.
Although there is still research required to confirm the efficacy of the model, without doubt training on 3D heart models offers great opportunities for training and can potentially improve patient safety in the near future. 3D model-based training is currently being evaluated for implementation in the national German training programme in paediatric cardiology.

What inspired you to work in the field of 3D medical printing for training purposes?
Hopfner: I was inspired by the people I met during my studies and work as a medical engineer, especially the ones outside of my field of expertise, ie, the physicians. Medical engineers should always seek for a close collaboration with physicians to develop medical applications exactly according to their needs. Trying to understand the physicians’ language and way of thinking, but at the same time to explain technical issues in a way that they understand what is possible and feasible makes my job so interesting.
Nagel: I was initially introduced to 3D printing and medical technologies during my studies. The fascinating aspect about my work with 3D printing is its diversity: on the one hand, the theoretical design on the computer, on the other hand the practical 3D printing process with a 3D heart as a result. Due to the increasingly personalised treatment of patients, I think that 3D printing should not only be offered as a service by companies, but should also be implemented directly in hospitals.
Haas: For me, education and training are extremely important. My goal is to improve the educational programme for future paediatric cardiologists – first in Germany and then worldwide, for example in Ethiopia, Mozambique, and Malawi. I want to do this by implementing hands-on 3D model training as a gold standard in the training programme of students in this field.
How are you planning to evaluate your training model in a real patient setting?
Trainees should first complete training on 3D heart models with visible improvement of radiation time during the procedure. This radiation time can then be compared to the radiation times measured during consecutive procedures on real patients.
What other applications could the 3D printed heart model have?
3D models can be used in patient education, anatomy training, preparation for surgery and interventions, simulation of interventions, surgery and surgical outcome, and the design of patient-specific medical devices. We already provide professional training courses to other hospitals and applications in Munich, Vienna, and Freiburg, but we want to expand on this and include other regions, with a special focus on Ethiopia (Mekelle / Addis Abeba).












