Perturbations of the early gut microbiome (dysbiosis) arising from antibiotic exposure, C-section, western diets, and formula feeding may affect later life risk for complex immune disorders like inflammatory bowel diseases (IBD). The research team led by Dr Eugene B. Chang (University of Chicago) and Dr Jun Miyoshi (Kyorin University) finds that key microbes essential to immune development are often missing in early life dysbiosis. Reintroduction of these microbes in early life (but not later in life) successfully restores development of the gut microbiome, immunity, and health. Their experimental findings highlight the importance of identifying early life dysbiosis and introducing timely interventions as part of future best practices.
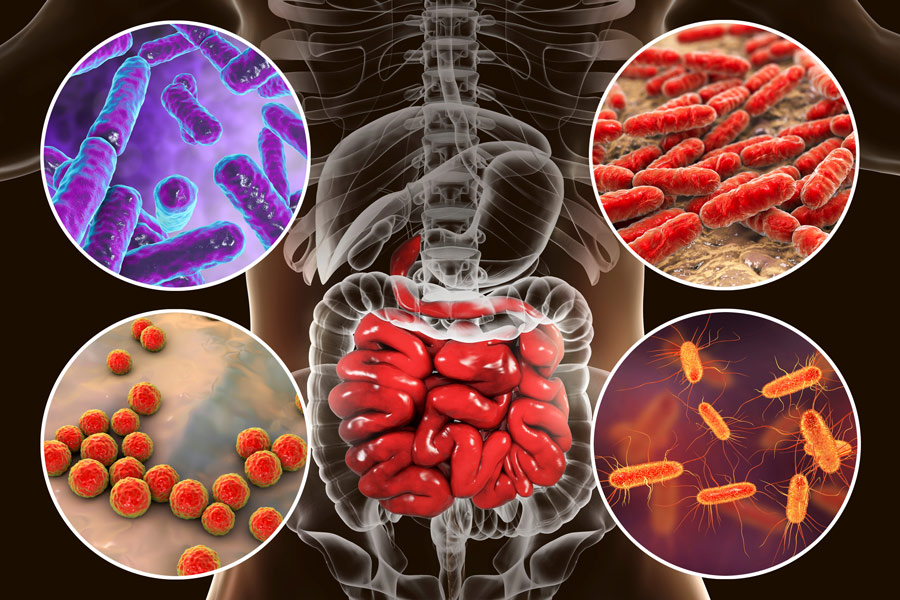
Inflammatory bowel diseases (IBD) such as ulcerative colitis and Crohn’s disease are chronic but manageable conditions. In modern times, they have been increasing in incidence at an alarming rate. Numerous factors play a role in the development of these conditions, including the environment, genetics, gut microbes, and early life imbalances in the gut microbiome (called dysbiosis) resulting from exposure to antibiotics or to the impact of formula feeding, malnutrition, or overnutrition. As a consequence, ‘health-essential’ microorganisms and the gut environment or ecosystem that they naturally inhabit (commonly referred to as the ‘microbiome’ – from the ancient Greek ‘mikrós’ [small] and ‘bίos’ [life]) can be severely disturbed and have both short or long-term health implications, e.g. increased risk of developing IBD (Miyoshi et al, 2021a; Gevers, et al Cell Host & Microbe 15, 382–392, 2014).
These implications have been highlighted over several different research areas – for example, the fecal microbiota of vaginally delivered versus Caesarean section (C-section) infants are different (Oliphant, et al, Gut Microbes), the former having a higher fecal abundance of Bacteroidota and Methanobacteriaceae compared to C-section delivered infants. Additionally, a 2021 study in Nature demonstrated that neonatal (new-born) exposure to antibiotics was associated with decreased abundance and diversity of the babies’ gut microbiome up to 2 years of age, and antibiotic use during the first 6 years of life is associated with higher Body Mass Index (BMI) later in life (carrying potentially severe implications associated with obesity). However, while clinical studies have reported associations between early life gut dysbiosis and later life disease risk, proof of concept and mechanistic insights are lacking.
“The healthy development of the early life gut microbiome sets the stage for proper host immune development and lower risk for IBD.”
The importance of the early life gut microbiome to development
Signals from the early life microbiome are essential for proper immune development and when perturbed can potentially affect health and disease states later in life, the latter including immune and metabolic disorders. During early life, an individual’s immune system learns what is ‘self’ so that it does not react to the body’s own cells. In this regard, the trillions of health-promoting microbes that live in our gastrointestinal tracts are also ‘self’ and tolerated by our immune system in a symbiotic relationship that has co-evolved over thousands of years. The educational process for the immune system occurs and is set in early life, after which immune cells can provide protection by reacting to cells and microbes it has not seen before. Thus, improper education of the immune system by an early life gut dysbiosis has been hypothesised to lead to disease-triggering responses later in life, particularly in genetically susceptible individuals/hosts. To determine if proof of concept could be demonstrated and to gain mechanistic insights, the team led by Dr Eugene B. Chang (University of Chicago) and Dr Jun Miyoshi (now at Kyorin University, Tokyo) took an experimental approach to test this hypothesis in genetically susceptible IL-10 gene deficient mice that are at risk for development of colitis (Miyoshi et al, 2021a).
The Chicago research team found that the antibiotic-induced early life gut dysbiosis lacked many ‘keystone’ microbes that were essential to the development of host immunity. This in turn was associated with increases in severity and incidence of colitis in later life. These observations closely parallel clinically observed associations and were later confirmed by another group (Schulfer, et al). Furthermore, they demonstrated that the engraftment of a vital missing keystone strain into the early life gut dysbiosis resulted in a significant decrease in the incidence and severity of colitis. In contrast, the engraftment of the same strain into the antibiotic-induced gut dysbiosis of adult mice does not have this protective effect (Miyoshi et al, 2021a). Thus, the intervention must be performed during a critical window in early life when the host immune system is still receptive to conditioning (Miyoshi et al, 2021a; Miyoshi et al, 2017). These findings underscore the importance of a judicious use of broad-spectrum antibiotics during late-term pregnancies or the neonatal period (Miyoshi et al, 2021a).
Studies of human subjects are still very limited and very difficult to conduct over the span of decades. Consequently, there are no reliable indicators to predict risk for developing IBD. In order to make significant advances in the field of human IBD, scientists still need to identify functional metrics which are more informative of potential impact of gut microbiomes to their host and may be useful for predicting future disease risk (Miyoshi et al, 2021b).
Microbiota pathways of nitrogen metabolism as predictive markers
A promising area to start with might be the nitrogen metabolism pathways. Within weeks after new offspring were born, Drs Miyoshi, Lee, Chang, and colleagues traced the differences between the functional (metagenomic) pathways of microbiota of mice that developed colitis later in life versus those that remained disease free. They found that bacterial nitrogen flux is associated with the incidence of overt colitis, where ammonia biosynthetic pathways were much more highly expressed in the mice with IBD than the ones without. The researchers opined that these types of markers can be useful predictors of risk for IBD in humans (Miyoshi et al, 2021b) in two ways. First, changes or imbalances in microbial metabolism and metabolites can set the stage whereby the host immune system is activated to cause disease. Second, the gut microbiome is highly sensitive to its environment and exhibits adaptive changes that can be detected as harbingers of clinical disease. In essence, the gut microbiome serves as the ‘canary in the coal mine’ where changes in its membership and function are early indicators of risk or development of diseases like IBD.
The early life microbiome provides key signals and factors that are essential for proper development of host immunity, an educational process that takes place in the first year or two of life. Correction of imbalances in the early life gut microbiome arising from dietary, environmental, and pharmacological factors can potentially restore gut microbial and immune development and lower risk for complex immune disorders such as inflammatory bowel diseases. Development of reliable markers and indicators of gut microbial health or unhealth will lead to next generation of clinical tools for risk assessment, precision interventions, and monitoring the health of an individual.
References
- Miyoshi J, Miyoshi S, Delmont TO et al (2021a) Early-life microbial restitution reduces colitis risk promoted by antibiotic-induced gut dysbiosis in Interleukin 10 absent mice. Gastroenterology. Vol. 161. P. 940-952. doi.org/10.1053/j.gastro.2021.05.054
- Miyoshi J, Lee STM, Kennedy M, et al (2021b) Metagenomic alterations in gut microbiota precede and predict onset of colitis in the IL10 gene-deficient murine model. Cellular and Molecular Gastroenterology and Hepatology. Vol. 11. P. 491-502. doi.org/10.1016/j.jcmgh.2020.08.008
- Kaitlyn Oliphant, Mehneez Ali, Mark D’Souza et al (2021) Bacteroidota and Lachnospiraceae integration into the gut microbiome at key time points in early life are linked to infant neurodevelopment, Gut Microbes, 13:1, 1997560 doi.org/10.1080/19490976.2021.1997560
- Miyoshi J, Bobe AM, Miyoshi S, Huang Y, Hubert N, Delmont TO, Eren AM, Leone V, Chang E (2017) Cell Reports. Vol. 20. P.491-504.
- Gevers D, Kugathasan S, Denson LA, Vazquez-Baeza Y, Van Treuren W, Ren B, Schwager E, Knights D, Song SJ, Yassour M, et al. The treatment-naive microbiome in new-onset Crohn’s disease. Cell Host Microbe. 2014; 15:382–392. [PubMed: 24629344]
10.26904/RF-140-2357174705
Research Objectives
Dr Eugene B. Chang and Dr Jun Miyoshi explore the impact of altered or dysbiotic early life gut microbiomes as risk factors for inflammatory bowel diseases and the importance of rebalancing the dysbiosis in early life to achieve proper immune development and lower risk for disease later in life.
Funding
NIDDK RC2DK122394-02; NIDDK R01DK47722, Gastrointestinal Research Foundation of Chicago; NIDDK P30 DK042086
Collaborators
Jun and Sawako Miyoshi (Kyorin University, Tokyo); Vanessa Leone (UWisconsin-Madison); Candace Cham (UChicago), A. Murat Eren (UChicago)
Bio

Dr Chang is the Martin Boyer Distinguished Professor of Medicine, Director of the Microbiome Medicine Program, and physician-scientist at the University of Chicago

Dr Miyoshi is Associate Professor and physician-scientist at the Kyorin University (Tokyo). Both are experts in the study of host-gut microbiome interactions in health and disease.
Contact
Eugene B. Chang MD
Department of Medicine
900 E 57th Street
Knapp Center for Biomedical Discovery (Rm 9130)
University of Chicago
Chicago, IL 60637
E: echang@medicine.bsd.uchicago.edu
T: 773-702-6458
W: www.changlab.uchicago.edu
W: www.mmp.bsd.uchicago.edu
Jun Miyoshi, M.D., Ph.D.
Associate Professor
Department of Gastroenterology and Hepatology
Kyorin University School of Medicine
6-20-2 Shinkawa, Mitaka-shi, Tokyo Japan 181-8611
T: +81-422-47-5511 ext. 3656
FAX: +81-422-71-5381
E: jmiyoshi@ks.kyorin-u.ac.jp










