- Migrant Pacific Island communities experience higher rates of mental illness than do the general population.
- Current mental health service delivery models are insufficient in addressing these issues.
- At the University of Waikato, Associate Professor Sione Vaka has harnessed the talanoa approach, a traditional research method practiced across Pacific Island nations.
- He aims to better understand the needs of a Pacific-centred mental health service and achieve equitable outcomes.
In Aotearoa/New Zealand, migrant Pacific Island communities experience higher rates of mental illness than do the general population. However, current mental health service delivery models in Aotearoa/New Zealand, Tonga, Fiji, and Niue are insufficient in addressing the high prevalence of mental illness among such communities. At the University of Waikato, and with support from the Health Research Council of New Zealand, Associate Professor Sione Vaka has harnessed the talanoa approach, a traditional research method practiced across Pacific Island nations, to better understand the needs of a Pacific-centred mental health service and develop a new model, the ūloa model, to improve Pacific health and healthcare provision.

The talanoa approach focuses on storytelling within formal and informal community groups. When the stories, lived experiences, and histories of the community members are drawn together, comprehensive understanding of a topic from a multitude of viewpoints can be achieved. To identify the barriers to effective mental health service provision, 30 talanoa were conducted in Aotearoa/New Zealand (Auckland), Fiji, Niue, and Tonga, including both individual and group talanoa. The results revealed six key themes relevant the provision of effective mental health services to Pacific Island communities.
1. Stigma and cultural barriers to mental health services
Many Pacific peoples face significant stigma and cultural barriers when seeking mental health services. These barriers often stem from traditional beliefs and societal norms that view mental illness as a taboo subject. Moreover, there was a feeling among some community members that mental illnesses were symptomatic of social and environmental problems. In many cases, the stigma attached to mental illness is self-imposed by the sufferer. An avenue to address this issue comes in the form of traditional healers, who are sometimes called upon to live with the affected family/person while they follow a journey towards healing.
2. Fragmentation of mental health services
Current mental health services are often fragmented and lack coordination, making it difficult for Pacific peoples to navigate the system and receive comprehensive care.
3. Role of faith and community support
Faith and community support play a crucial role in the mental well-being of Pacific peoples. Churches and community groups often provide essential support networks and can be pivotal in mental health interventions.
Mental health service providers should harness this community structure; for example, through mental health awareness programmes run through church groups and kava circles. In particular, when run in collaboration with influential community leaders, such gatherings offer a power tool to both gather and disseminate knowledge on mental health issues.
4. Barriers to accessing professional mental health services
There are numerous barriers to accessing professional mental health services, including language barriers, lack of culturally competent practitioners, and financial constraints.
5. Need for a holistic and culturally embedded model of care
There is a strong need for a holistic approach that integrates traditional Pacific healing practices with modern clinical care. This model should be culturally embedded, and both respecting of and incorporating Pacific values, beliefs, and practices. Continued focus on physiological or biomedical models of mental distress to the exclusion of biopsychosocial factors and traditional concepts, such as loto (soul), ongo (emotional context of a person’s experience), and atamai (the mind), can negatively shape a service user’s interpretation of the experience.

Other examples include the recognition of metaphors and their importance in communication (for example, portraying mental illness by describing tangible objects that have sustained damage), particularly within Tongan communities. The importance of supporting not just individuals with mental health issues, but also the whole household, with harmony (or napanapangamalie), including domestic harmony, being a cornerstone of good mental health in Pacific Island communities. Finally, recognition of the role of spirits and deities, specifically the displeasure of spirits and deities, in imbuing mental distress.
6. Mental health workforce challenges
The mental health workforce faces challenges such as a shortage of culturally competent practitioners and high turnover rates. There is a need for more training and support for mental health professionals working with Pacific communities. By prioritising training and development in cultural competence, the mental health workforce can be better equipped to meet the needs of Pacific peoples.

In addition, another concept to emerge from the process was that of fakataha, or ‘working together’, with a need for modern medical practitioners to work together with traditional healers to achieve optimal results. However, critically, community members also emphasised the importance of self-determination in mental healthcare, a radical departure from doctor-led modern medicine. All participants within the process (mental health service provider, traditional healer, family, and community) contribute unique expertise in a shared or interchangeable role of toutai (or decision maker), ultimately harnessing the service user with the tools to be the toutai themselves.
A fundamental shift for mental health delivery
The findings of this research underscore the critical need for culturally responsive mental health services tailored to the unique needs and perspectives of Pacific communities. Inadequacies in the current system are largely due to systemic fragmentation, cultural stigma, and barriers to accessing professional care.
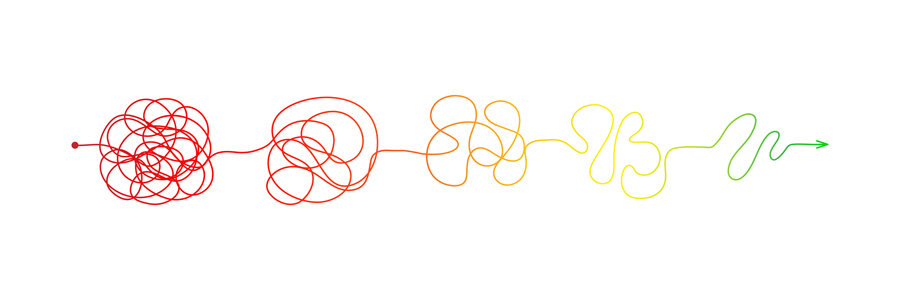
Rather than perpetuating existing methods and expecting different outcomes, a fundamental shift in the foundation and delivery of mental health services for Pacific communities is needed. Such a model should be grounded in Pacific ethnic knowledge, worldviews, and practices, ensuring that mental health services are not only culturally appropriate but ensure more effective, meaningful, and equitable outcomes for Pacific peoples.
Do any mental health service providers currently employ traditional healers as part of their practice? If not, would this be an option? Or do traditional healers work better outside of the medical structure?
It would be great to include traditional healers in the medical structure. This is very much needed as we have been trying different methods with little inclusion of cultural intervention and method. The current system does not work for Pacific people. Too clinical, cold, aggressive and it ignores cultural perspectives which can cause cultural injuries. This creates a lack of trust from Pacific people in the health services.










